CITA ESTE TRABAJO
Plaza Fernández A, Rodríguez Mateu A, Valdenebro Cuadrado G, Diéguez Castillo. Beyond the intestine: acute pancreatitis secondary to eosinophilic gastroenteritis.RAPD 2025;48(5):197-199. DOI: 10.37352/2025485.5
Clinical case
A 33-year-old male with no relevant personal history presented to the emergency department with severe abdominal pain in the mesogastrium and diarrhea without pathological findings. Laboratory tests revealed leukocytosis with marked eosinophilia, and computed tomography (CT) showed thickening of the duodenum and jejunal loops with mesenteric engorgement and reactive lymph nodes consistent with duodenoyejunitis (Figure 1). The study was completed with gastroscopy and colonoscopy, revealing cobblestone mucosa and multiple fibrinous ulcerations in the duodenum, which were biopsied. Pathological examination showed an increase in eosinophils forming microabscesses, leading to a diagnosis of eosinophilic gastroenteritis (Figure 2). Twenty-four hours after admission, the patient showed clinical worsening and hyperamylasemia, requiring an urgent CT scan to rule out perforation of a hollow viscus, but findings of acute pancreatitis were observed (Figure 3). He was discharged and later returned to the emergency room complaining of pain. A CT scan was performed, revealing radiological findings consistent with acute pancreatitis. After ruling out other conditions (Table), this was related to the eosinophilic inflammatory intestinal process. Given the suspected diagnosis, treatment with intravenous corticosteroids was initiated, resulting in progressive clinical improvement and resolution of the symptoms.
Figure 1
CT image showing distension of jejunal loops approximately 3 cm in caliber, located in the left hypogastrium and umbilical region with intramural fluid content and slight wall thickening. Adjacent reactive-appearing lymph nodes in the mesentery. Minimal amount of free fluid in the pelvis.
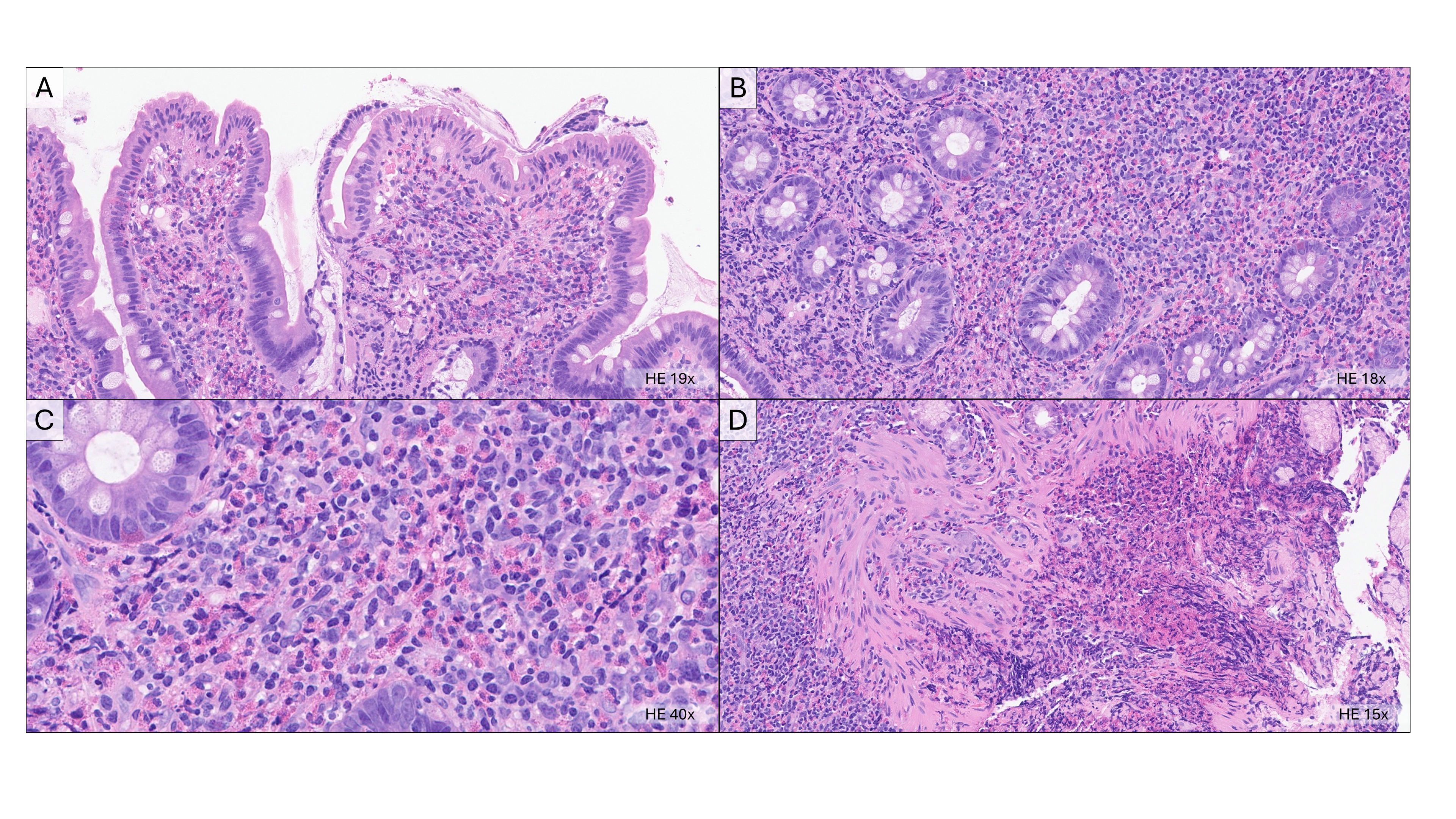
Figure 2
A-C: Duodenal mucosa with reparative-regenerative characteristics, with preserved architecture and villous height. The lamina propria shows a diffuse mixed inflammatory infiltrate composed predominantly of eosinophils, as well as lymphocytes, plasma cells, and neutrophils in smaller proportions. Groups of eosinophils forming microabscesses (accumulations of 4 or more eosinophils) are observed. D: Inflammatory infiltrate in the lamina propria, lymphoplasmacytic and mainly eosinophilic, reaching the muscularis mucosae and converging to form an extensive eosinophil microabscess. Duodenal mucosa in the vicinity preserved with reparative-regenerative changes.
Figure 3
CT image showing diffusely thickened pancreas with rarefaction of peripancreatic fat, changes suggestive of acute edematous-interstitial pancreatitis.
Table 1
Summary of the patient's laboratory abnormalities described in the text.
Discussion
Eosinophilic gastroenteritis (EGE) is a rare condition characterized by eosinophilic infiltration of the gastrointestinal tract in the absence of secondary causes such as parasites, drugs, or neoplasms. Its manifestations depend on the layers of the intestinal wall involved and may affect the pancreas to a limited extent secondary to obstruction of the biliary system. Imaging tests often reveal thickening of the duodenal wall, which is also observed by endoscopy, with the diagnosis being confirmed histologically by the presence of eosinophilic infiltrate in the gastric and/or intestinal tissue. This case emphasizes the importance of considering EGE as a cause of acute pancreatitis in patients with eosinophilia and digestive symptoms, especially when other common causes have been ruled out.

 Descargar número completo
Descargar número completo Download full issue
Download full issue