CITA ESTE TRABAJO
Rodríguez Mateu A, Fernández Carrasco M, Plaza Fernández A, Sánchez García O. Chronic diarrhea in an hiv patient: gastrointestinal involvement by histoplasma capsulatum. RAPD 2025;48(3):114-116. DOI: 10.37352/2025483.5
Introduction
Histoplasmosis is a systemic granulomatous mycosis caused by infection with the fungus Histoplasma capsulatum. It is an endemic infection in tropical regions, with special incidence in immunocompromised patients, particularly those with advanced stages of human immunodeficiency virus (HIV) infection[1].
Exclusive gastrointestinal involvement is infrequent and, in the absence of treatment, leads to high mortality. Its presentation is usually subacute, with non-specific symptoms, especially chronic diarrhea and constitutional syndrome[2]. The most common location is the ileocecal area, where it can manifest in three endoscopic patterns: stenotic, ulcerative and edematous.
Given the rarity of this entity in our environment, and with the aim of emphasizing the importance of differential diagnosis in immunocompromised patients with chronic diarrhea, we present the case of a male with previously undiagnosed HIV infection, who presented with duodenitis and granulomatous ileocolitis due to Histoplasma capsulatum.
Clinical Case
A 26-year-old man from Colombia, with no known allergic history, recently diagnosed with HIV infection stage C3, in antiretroviral treatment. He consulted for diffuse abdominal pain, predominantly in the right flank, of 4 months of evolution, associated with semi-liquid diarrhea (4-5 stools per day), asthenia, unquantified fever, hyporexia and weight loss of 20 kg.
His personal history included syphilis of undetermined duration and occult hepatitis B. He was not immunized against hepatitis B. he had no immunization against hepatitis A, hepatitis C, SARS-CoV-2, pneumococcus or human papillomavirus.
Physical examination revealed cachexia (BMI: 14.5 kg/m²), with no relevant findings on cardiorespiratory auscultation. The abdomen was painful on palpation in the right flank, with no signs of peritoneal irritation, masses or visceromegaly.
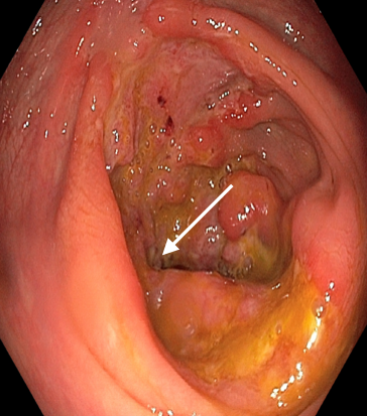
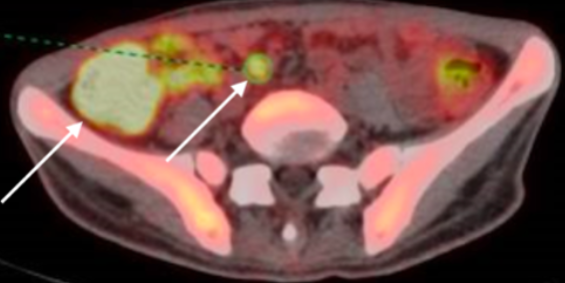
Complementary tests showed bicytopenia (Hb 8.8 g/dL; leukocytes 4,800/mm³), CD4+ lymphopenia of 50/mm³, viral load of 26,000 copies/mL and C-reactive protein 7.8 mg/L. Colonoscopy showed deep ulcers in the cecum, ascending colon and ileocecal valve (Figure 1), findings confirmed by contrast-enhanced abdominopelvic CT, which revealed thickening of the right colon and terminal ileum, as well as locoregional and periduodenal adenopathies. The PET-CT scan showed hypermetabolism in the duodenum, cecum and right colon (Figure 2).
Figure 2
Hyperenhancement at the level of the duodenum (medial) and right colon (lateral) in PET-CT study.
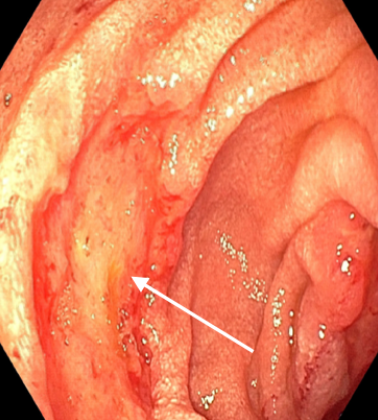
Suspecting duodenal involvement, gastroscopy was performed, showing erythematous and inflamed mucosa in the second duodenal portion, with fibrin-covered ulcers (Figura 3). Biopsies confirmed the presence of Histoplasma capsulatum by positive Grocott staining.
Induction antifungal treatment was started with intravenous liposomal amphotericin B (4 mg/kg/day) for 14 days, followed by oral itraconazole (200 mg/8 h for 3 days and then 200 mg/12 h for at least 12 months). However, one month after starting treatment, the patient presented postprandial abdominal pain with vomiting and no new diarrhea. Gastrointestinal transit showed interruption of passage at the duodenal knee level, compatible with obstruction due to postinflammatory fibrosis (Figure 4), so gastrojejunal bypass with resection of the duodenum and ileum and entero-enteric anastomosis was performed.
Postoperative evolution was favorable, with no immediate or delayed complications. Currently, the patient remains asymptomatic and under ambulatory follow-up, with no evidence of recurrence.
Discussion
Gastrointestinal involvement by Histoplasma capsulatum is an atypical form of presentation of this endemic mycosis, especially in immunocompromised patients from endemic areas such as Central and South America, Southeast Asia and certain areas of Africa[1]. The nonspecific clinical features, together with endoscopic findings that may mimic other infectious or inflammatory colitis, make its initial diagnosis difficult.
The differential diagnosis should include intestinal tuberculosis, due to its high prevalence in this population, as well as inflammatory bowel disease[2]. Diagnostic confirmation requires identification of the fungus in tissue samples by histological techniques and culture[3].
Although it is an uncommon entity in Europe, its inclusion in the diagnostic algorithm is essential in immunosuppressed patients with chronic diarrhea and compatible epidemiological history. The prognosis, without treatment, is severe, but with appropriate antifungal therapy, the outcome is usually favorable[4].
This case highlights the need for a multidisciplinary approach - gastroenterology, microbiology, surgery - given the potential variability of the clinical picture and the resulting complications, such as postinflammatory intestinal stenosis. Individualization of treatment is key, adapting it to the extent of the disease and the patient's comorbidities.

 Descargar número completo
Descargar número completo Download full issue
Download full issue