CITA ESTE TRABAJO
Fernández Carrasco M, Plaza Fernández A, Navarro Moreno E, Anguita Montes F, Gálvez Miras A. Chronic ischemic gastropathy as an unusual cause of abdominal pain. RAPD 2024;47(5):192-194. DOI: 10.37352/2024474.5
Clinical case
We present the case of a 57-year-old male smoker with a history of arterial hypertension, dyslipidaemia and revascularised ischaemic heart disease, who was admitted for abdominal pain in the mesogastrium that intensified after eating, of two months' duration, associated with anaemia and weight loss.
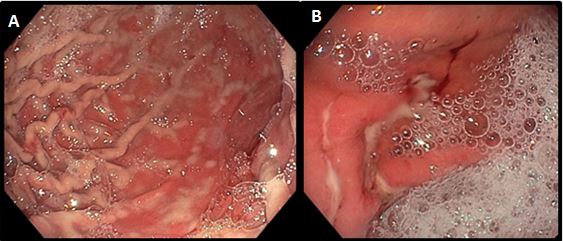
We present the case of a 57-year-old male smoker with a history of arterial hypertension, dyslipidaemia and revascularised ischaemic heart disease, who was admitted for abdominal pain in the mesogastrium that intensified after eating, of two months' duration, associated with anaemia and weight loss. Upper gastrointestinal endoscopy was performed with findings of linear fibrinous ulcers in the antrum, with a change in the colour of the gastric mucosa after insufflation, showing whitish areas suggestive of areas of hypoperfusion (Figure 1). The study was completed with computed tomography angiography showing evidence of calcified atheromatous disease leading to severe stenosis at the origins of the celiac trunk and superior mesenteric artery (Figures 2 and 3).
Figure 1
Upper endoscopic images of: gastric chamber at maximum insufflation with pale gastric fold mucosa (A) and fibrinous linear ulcers (B).
Figure 2
Computed tomography angiography showing aortic calcified plaque at the exit of the celiac trunk and superior mesenteric artery.
The patient underwent surgery to recanalise the celiac trunk and implant a stent in the superior mesenteric artery, with resolution of the clinical condition that precipitated admission.
Discussion
Due to the rich collateral circulation from the branches of the celiac trunk and the superior mesenteric artery, gastric ischaemic pathology is rare. The aetiology is in almost all cases atheroembolic[2], which has led to an increase in its incidence in recent decades, due to the ageing of the population and the rise of cardiovascular diseases.
Clinical manifestations may occur in a larval form in chronic cases, in which postprandial pain is the predominant symptom, and may be accompanied by anaemia due to gastrointestinal bleeding and weight loss due to fear of ingestion. However, in acute cases of abrupt occlusion of one of the main branches, fulminant gastric ischaemia occurs with a fatal short-term prognosis and high mortality[1],[4].
Treatment, whenever possible, is early revascularisation, preferably percutaneous endovascular angioplasty with stent placement to prevent restenosis of the same segment[5].
El tratamiento, siempre que sea posible, es la revascularización precoz, preferiblemente por vía percutánea endovascular mediante angioplastia con colocación de stent para prevenir la reestenosis del mismo segmento[3].
This is therefore a case that highlights the importance of the differential diagnosis of abdominal pain, with clinical suspicion of this entity being essential in patients with suggestive symptoms and established cardiovascular risk factors, as it has been shown that early revascularisation significantly improves survival rates6.

 Descargar número completo
Descargar número completo Download full issue
Download full issue