CITA ESTE TRABAJO
Villegas Pelegrina P, Navarro Moreno E, Delgado Maroto A. Obscure gastrointestinal bleeding, a diagnostic challenge. RAPD 2024;47(4):160-162. DOI: 10.37352/2024474.4
Introduction
A persistent or recurrent bleeding from the gastrointestinal tract, in which no origin is identified after a complete and quality gastroscopy and colonoscopy, is known as obscure gastrointestinal bleeding (OGIB). It is considered overt if the bleeding is visible in the form of rectorrhagia, haematochezia or melena, and occult when found by positive faecal occult blood test and/or iron deficiency anaemia. Only 5% of gastrointestinal haemorrhages have their origin in the small intestine, posing a diagnostic-therapeutic challenge due to the greater number of complementary tests required, thus increasing the expenditure of healthcare resources. We present a clinical case of a gastrointestinal haemorrhage in which it was necessary to go beyond gastroscopy and colonoscopy, requiring a multidisciplinary approach.
Clincal case
72-year-old male with a history of type 2 diabetes mellitus, dyslipidaemia, COPD and sigmoid diverticulosis. He came to the emergency department for an episode of rectorrhagia of two days' evolution, associated with syncope and food vomiting. He denied taking anti-inflammatory drugs, anticoagulants or toxic habits. On arrival he presented haemodynamic repercussions and anaemisation of five haemoglobin points. After haemodynamic resuscitation and red blood cell transfusion, gastroscopy revealed no signs of bleeding or lesions. Given the persistence of rectorrhagia and haemodynamic instability, a CT angiography was performed, but no contrast leakage was observed.
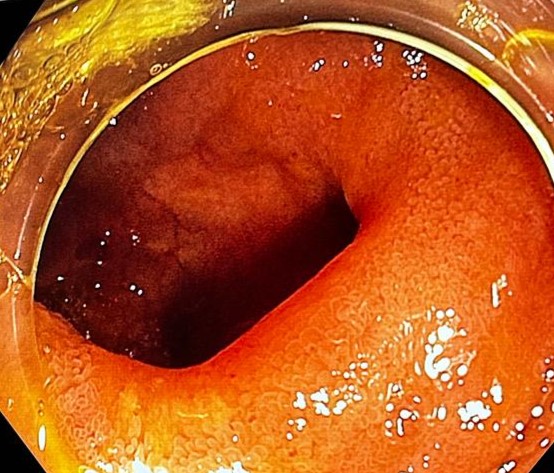
The patient was then prepared for colonoscopy, which was incomplete due to the presence of clots and fresh blood, and was repeated, this time complete, with no lesions observed. Subsequently, arteriography of the mesenteric arteries was performed, observing signs suggestive of bleeding dependent on the jejunal branch, without being able to perform any occlusive procedure. An endoscopic capsule was administered, where active bleeding in the jejunum was suspected, and finally, an intraoperative endoscopic exploration was performed, and the colonoscope was advanced to the jejunum; and surgery performed a median laparotomy, identifying several diverticula located immediately distal to the angle of Treitz. On examination of the last diverticulum, a vessel was visible at the bottom, with no active bleeding at that time. The final treatment was resection of a segment of proximal ileum and distal jejunum encompassing several diverticula, after which there were no new signs of bleeding.
Discussion
75% of OGIB have their origin in the small intestine, the rest are upper or lower haemorrhages that go unnoticed. The most common aetiology is vascular ectasia, especially in patients over 40 years of age and those with multiple pathologies, although in young patients tumours or Meckel's diverticulum must be ruled out. Although there are various causes, the cause of our clinical case is uncommon: small bowel diverticula.
Management will depend on the patient's condition, as the number and aggressiveness of the interventions must be in accordance with the severity of the condition and the patient's baseline condition. Few cases reach the end of the diagnostic-therapeutic algorithm, and therefore intraoperative endoscopy is rarely necessary.
If the patient is stable, capsule endoscopy is administered to identify possible causes of bleeding in the small intestine, followed by enteroscopy, either diagnostic or therapeutic. If, on the other hand, haemodynamic instability is present, arteriography is performed, usually preceded by an angio-CT scan, which can be therapeutic by means of embolisation techniques. If interventional radiology fails to control the bleeding, a deep enteroscopy is performed, in some cases even intraoperatively, to locate the bleeding point with the help of surgery, performing a laparotomy and sliding the intestinal loop over the endoscope until the origin of the bleeding is located.

 Descargar número completo
Descargar número completo Download full issue
Download full issue