CITE THIS WORK
Valdés Delgado T, Rodríguez-Téllez M. Tratamiento endoscópico de las varices gástricas: ¿cuándo y cómo? RAPD 2024;47(3):116-122. DOI: 10.37352/2024473.3
Introduction
Gastric varices (GV) are present in approximately 20% of cirrhotic patients with portal hypertension (PH), with GV bleeding being less frequent than oesophageal variceal (EV) bleeding. However, when GVs bleed, they bleed more rapidly and profusely, leading to higher mortality (mortality rates of up to 45%), higher rates of treatment failure and thus rebleeding (rebleeding rates 35-90%)[1]. All this, added to the complexity of its pathophysiology and vascularisation, presents us with a diagnostic and, above all, therapeutic challenge.
In general, the risk factors for GV bleeding are: advanced liver disease (Child B-C), GV >5 mm, GV with red dots and their location, fundic varices (FV) have a higher risk of bleeding than the rest[2].
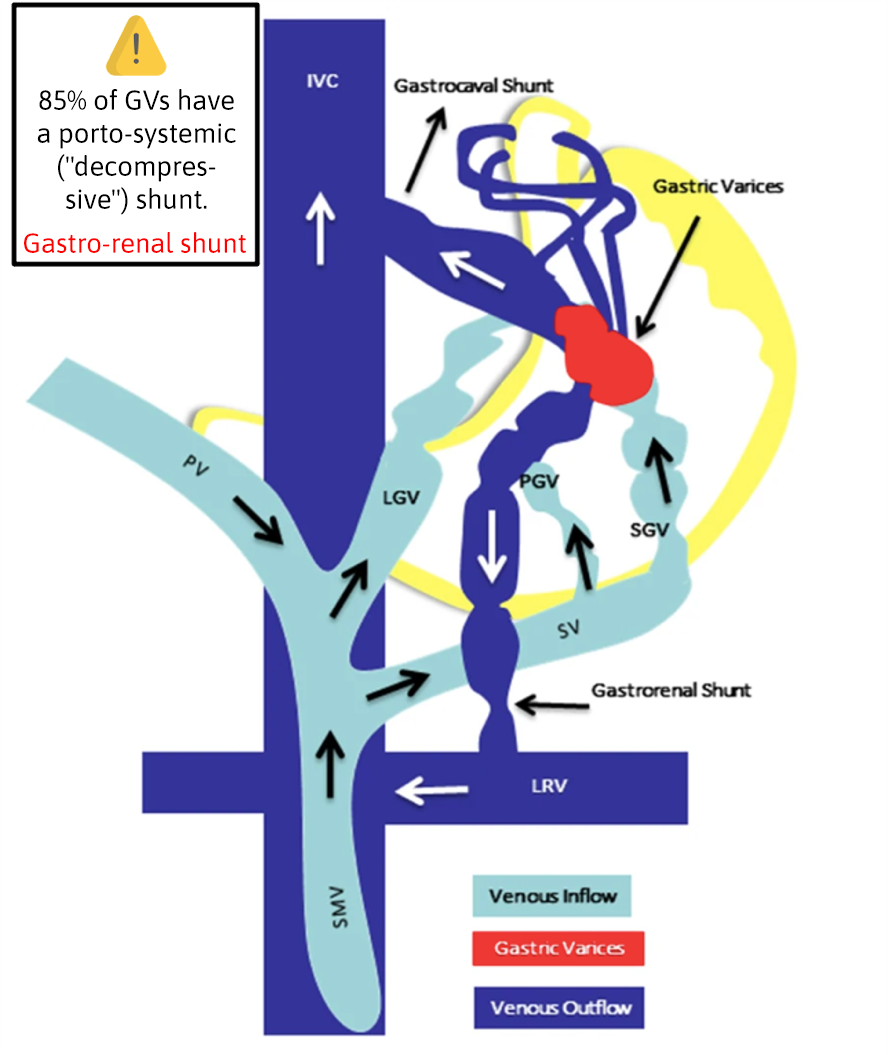
As for their pathophysiology, GVs are made up of an afferent, nutritive or inflow vein and an efferent or outflow vein. This efferent vein, in 85% of cases, is formed by a decompressive portosystemic shunt, to which the systemic complications of the most widely used treatment at present, the injection of cyanoacrylate, are attributed[3],[4] (Figure 1).
Classification
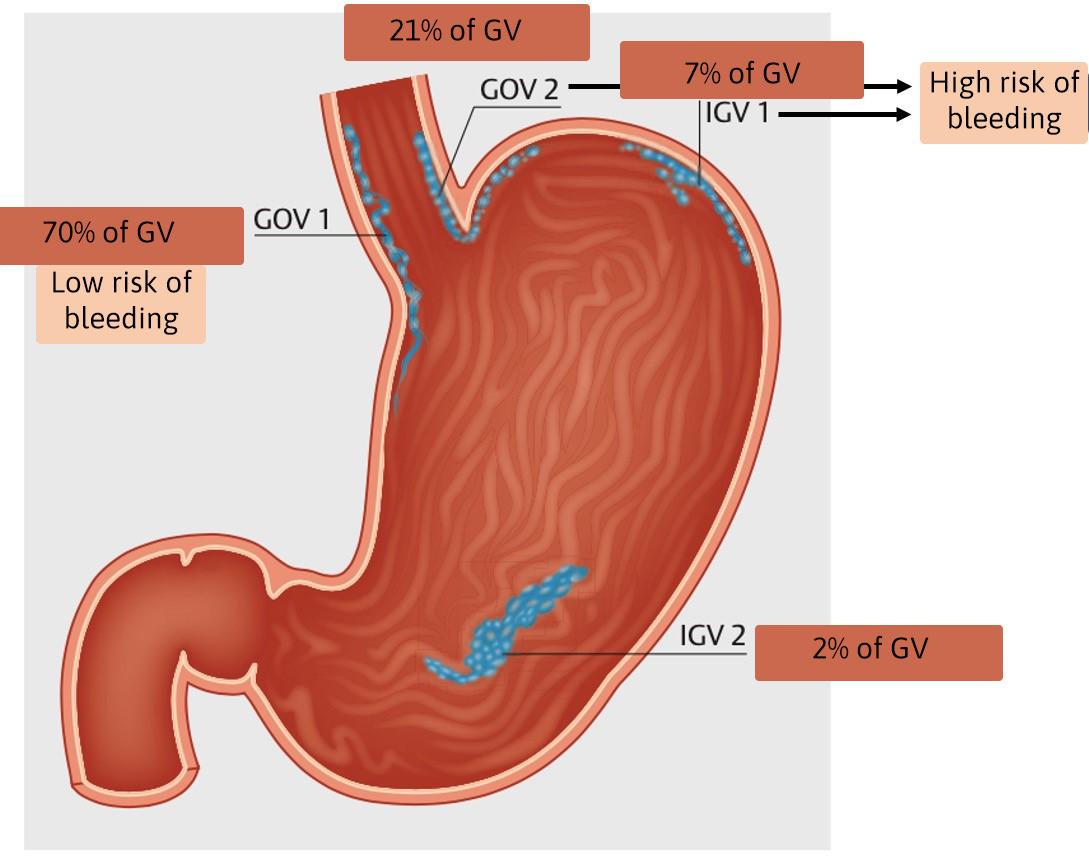
In order to be able to treat them correctly, it is essential to define and characterise them with criteria. There are several classifications[5],[6], but the one used in endoscopy and endorsed by Baveno VII[7], is the Sarin classification[1]. It divides them according to their location into oesophagogastric or "junctional" varices, type GOV-1 (extending towards the lesser curvature) and GOV-2 (extending towards the fundus); on the other hand, isolated gastric varices type IGV-1 (in the fundus) and IGV-2 elsewhere. The most frequent are GOV-1 (70% of GVs) and have a lower risk of bleeding. In contrast, IGV-1 and GOV-2 are less frequent but have a high risk of bleeding, and are the origin of GV bleeding in 60-70% of cases[7],[8] (Figure 2). EThese FVs are the focus of this controversy.
Available treatments
Depending on the scenario and the techniques available in each centre, we can apply one treatment or another.
1. CONVENTIONAL GASTROSCOPY
Elastic bands. Cyanoacrylate injection.
Sclerotherapy (ethanol, ethanolamine or polidocanol).
2. ECOENDOSCOPY
Cyanoacrylate injection.
Coil release.
Coil release + cyanoacrylate injection.
3. INTERVENTIONAL RADIOLOGY
TIPS (trans-jugular intrahepatic portosystemic shunt).
BRTO (Balloon-occluded retrograde transvenous obliteration).
Different clinical scenarios
1. Gastric varicose veins with active bleeding. Treatment is always necessary.
2. Gastric varices that have bled, but at the time of gastroscopy there is no active bleeding. The treatment to be applied is secondary prophylaxis.
3. Gastric varices that have never bled. The treatment we decide on is primary prophylaxis.
Treatment of active bleeding from gastric varices
Initial assessment, resuscitation and general measures
Management of these patients should be carried out in critical or intermediate care units, at least during the first hours.
Baveno VII supports a conservative transfusion strategy, aiming for a haemoglobin of 7-8 g/dL; and avoid routine transfusion of fresh frozen plasma or platelets.
Specifically, routine orotracheal intubation prior to endoscopy is discouraged, reserving the latter for patients with altered level of consciousness or active haematemesis.
Prevention of bacterial infection remains a priority objective and intravenous ceftriaxone (1g/24 h) remains the most commonly used option in clinical practice. Withdrawal of proton pump inhibitors is recommended once endoscopy confirms the variceal origin of the bleeding.
Specific pharmacological haemostatic therapy of acute bleeding consists of early administration of vasoactive drugs (terlipressin, somatostaine or octreotide) as early as possible, to be maintained for 2-5 days, in addition to endoscopic treatment in the first 12 h after stabilisation of the patient (or as soon as it is safe if instability persists). For these reasons it is considered essential that hospitals caring for patients with acute variceal haemorrhage have a gastroenterologist with experience in endoscopy available 24 hours a day[9].
Specific endoscopic treatment
Whenever there is active bleeding at the time of gastroscopy, some endoscopic treatment should be applied.
Endoscopic options currently available to treat acute GV bleeding include sclerotherapy, endoscopic band ligation (EBL) and cyanoacrylate injection. However, high-quality data for choosing the optimal strategy remain limited, with inconsistencies between trials regarding mortality, incidence of rebleeding and adverse events.
Several systematic reviews/meta-analyses[10]-[13] have evaluated the efficacy of cyanoacrylate injection for the treatment of GV bleeding and compared it with other endoscopic methods (sclerotherapy or EBL), with cyanoacrylate being superior in most outcomes, achieving better rates of immediate haemostasis and prevention of rebleeding.
Based on current evidence, clinical practice guidelines (ESGE and Baveno VII[7],[8]) recommend:
1. GOV-1 and IGV-2 type GVs can be treated the same as EVs with EBL.
2. GOV-2 and IGV-1 type GVs should be treated with cyanoacrylate injection by conventional gastroscopy, achieving high rates of immediate haemostasis and low rates of rebleeding. In addition to being effective, it is easy and safe to apply in an emergency.
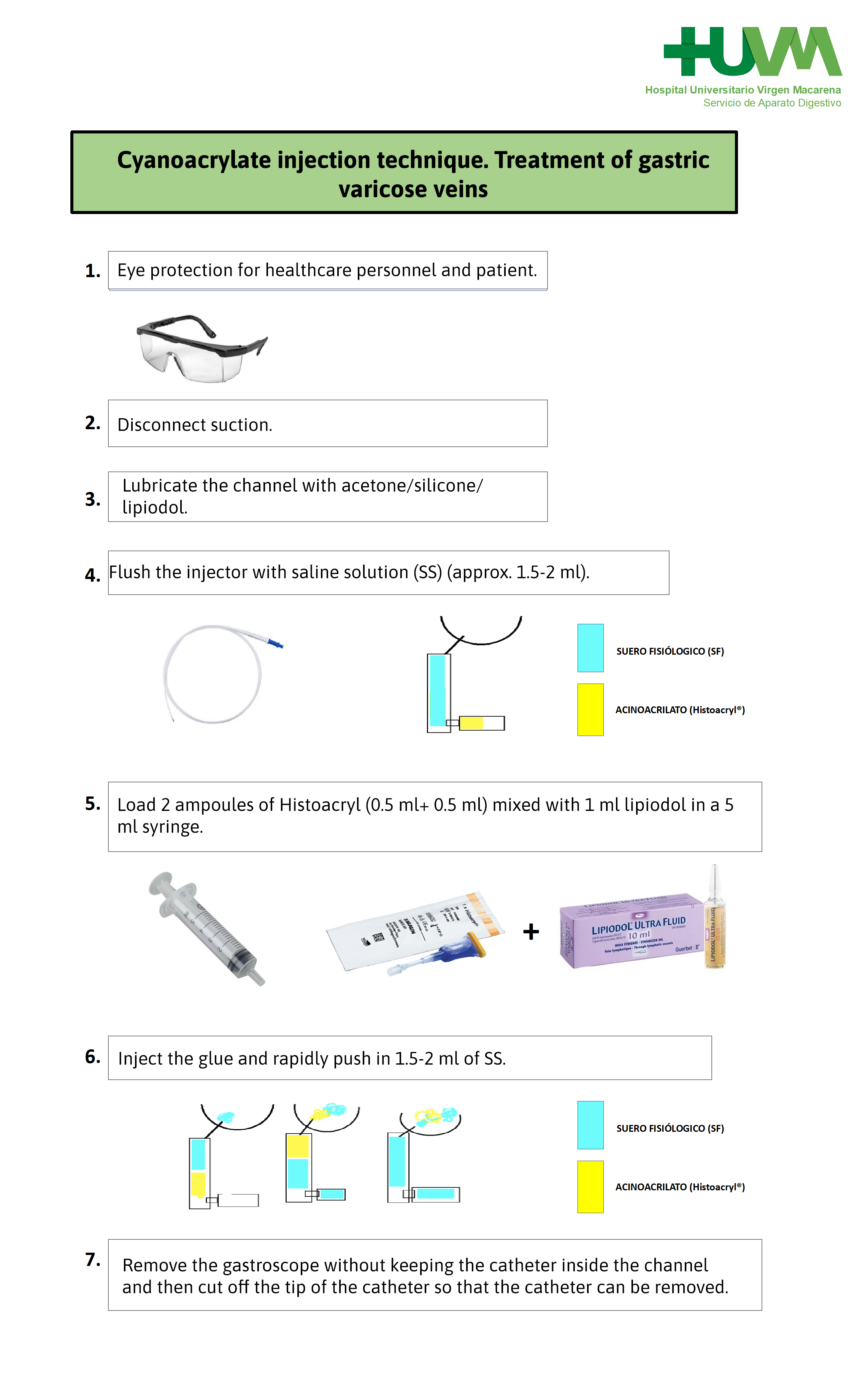
Cyanoacrylate is a tissue adhesive that polymerises rapidly on contact with blood and becomes a hard, acrylic material that will obliterate the varicose vein[3],[14]. In the United States it was approved by the FDA in 1998, but its use is restricted and few authorised centres are allowed to use it. Although it was first described in 1986 for the treatment of GVs by Soehendra, there are several ways of doing it and this is what makes the technique somewhat confusing and complex for endoscopists. For this reason, the endoscopy service of our hospital ( Virgen Macarena University Hospital) together with the nursing staff, have developed a protocol according to our availability and experience, explaining the whole process step by step (Figure 3).
1. Lubricate the channel with acetone/silicone/lipiodol.
2. Disconnect suction.
3. Flush the injector with saline solution (SS) (approx. 1.5-2 ml).
4. Load 2 ampoules of Histoacryl (0.5 ml+ 0.5 ml) mixed with 1 ml lipiodol in a 5 ml syringe.
5. Inject the glue and rapidly push in 1.5-2 ml of SS.
6. Keep the needle inside the catheter to avoid tissue impaction (adhesive).
7. Remove the gastroscope without keeping the catheter inside the channel and then cut off the tip of the catheter so that the catheter can be removed.
In addition to the preparation and care during injection, special precautions must be taken with cyanoacrylate, such as in large portosystemic shunts, cardiac septal defects or hepatopulmonary syndrome, due to the risk of symptomatic and severe embolism. Lipiodol is used to control the polymerisation time and, very importantly, as a contrast medium, a particularly useful advantage in cases of suspected embolisation. Although in most cases systemic emboli are asymptomatic, some studies describe up to 50% of these[15],[16],[17].
Other complications of this technique are the formation of post-injection ulcers or fistulas, as well as systemic infections. Special mention should be made of complications related to the equipment, such as adhesion of the glue to the lens or to the gastroscope channel.
All these drawbacks of direct injection of cyanoacrylate by gastroscopy can be minimised or even eliminated by echoendoscopically guided administration, which would also allow for coil release[15],[17].
The first time the echoendoscopy-guided coils release technique was performed to treat acute bleeding due to gastric varices was at Virgen Macarena University Hospital in Seville in 2010, by Romero-Castro et al.[15]. In 2011, Binmoeller et al.[18] described this same technique, combined with cyanoacrylate, achieving a 96% obliteration rate of gastric varices in a single treatment session, without clinical signs of embolization with cyanoacrylate. Since this initial study, multiple retrospective studies, two randomised clinical trials and systematic reviews/analyses have been published on this topic[19],[20], concluding that the treatment of acute GV bleeding is more effective and safe under endoscopic guidance and in combination (coils + cyanoacrylate).
Despite this evidence in the literature, for the moment, clinical practice guidelines[7],[8] do not strongly recommend this combined technique guided by echoendoscopy as the treatment of choice for acute GV bleeding. This may be due to the complexity of applying it in an emergency; these techniques are safer but only performed by expert personnel and are more expensive.
Where the recommendation for the combined echoendoscopy-guided technique is strong, on a par with the other options, is in secondary prophylaxis, which we will see later.
Persistent bleeding or early rebleeding of gastric varices
When endoscopic primary haemostasis fails or we have early recurrent bleeding we have to resort to the urgent salvage radiological techniques, TIPS or BRTO. There are very limited high level data comparing TIPS and BRTO in these situations[21],[22]. BRTO and TIPS have similar rates of technical success and adverse effects. TIPS is associated with higher rates of hepatic encephalopathy and BRTO with long-term aggravation of oesophageal varices. Due to the limited quality of comparative data, no specific selection criteria are currently available, therefore individualisation according to patient and centre experience is necessary.
Primary and secondary prophylaxis of gastric varices
Primary prophylaxis (GVs that have never bled) is performed in the same way and with the same criteria as EVs. When patients cannot receive non-selective beta-blockers (BBNS) (due to intolerance or contraindication), in the case of GOV-1 type GVs, they should be treated like EVs with EBL. However, in the case of FVs, type GOV-2 or IGV-1, to date there are no firm recommendations on the endoscopic treatment of FVs in patients with intolerance to BBNS. In fact, the ESGE suggests, with a weak recommendation and low evidence, that it is equally valid not to perform any treatment or to treat them, either with cyanoacrylate injection by gastroscopy or treatment by echoendoscopy with coils + cyanoacrylate, on a case-by-case basis, and if treated, in centres with experience in the technique[8].
In secondary prophylaxis (GVs that have bled at some point), GOV-1s are treated the same as EVs. For FVs, type GOV-2 and IGV-1, it is difficult to provide solid evidence-based recommendations due to the heterogeneity of previous research and the lack of uniform definitions or standardised outcomes. The available literature consists of case series, restricted cohort studies and a few small randomised trials, with significant selection biases[23]. Therefore, the ESGE recommends an individualised approach, based on patient factors and local experience for FV eradication therapies, considering endoscopic injection of cyanoacrylate +/- BBNS, combined treatment with coils + cyanoacrylate guided by echoendoscopy, TIPS placement or BRTO8. A recently published network meta-analysis[24] suggested that BRTO may be the best intervention to prevent FV rebleeding (secondary prophylaxis), while BBNS monotherapy cannot be recommended; however, direct comparative studies are much needed.
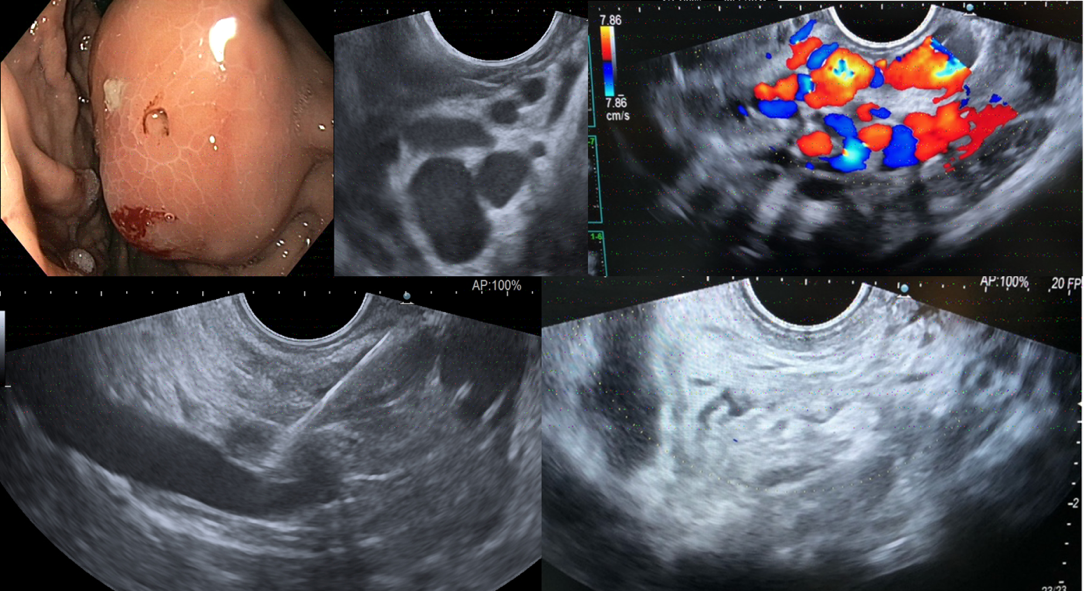
With regard to treatments guided by endoscopic ultrasound, the target is to puncture the nutrient vessel, the perforating vein, or, failing that, the varicose vein directly. In addition, this allows us to perform it when endoscopic vision is limited by bleeding, since with Doppler we can locate the vessels and the flow, and Doppler also allows us to check the cessation of flow when the varicose vein is obliterated (Figure 4). This can be done with different methods of obliteration: with cyanoacrylate alone, with coils alone, or with a combination of both. After a first GV treatment session, the next revision is recommended after 4-6 days and thereafter, as with EVs, every 2-4 weeks until complete GV obliteration is achieved[25]. The steps for cyanoacrylate injection and echoendoscopically guided coil placement are explained below.
Figure 4
Example clinical case Dr. Romero. Placement of coils in GOV-2 varix. Gastric varix with intense Doppler flow (figure 3). Injection of 6 coils (figure 4). Complete cessation of intravariceal flow (figure 5).
Echoendoscopy-guided cyanoacrylate injection technique:
1. 22G needle purged by glucosmon.
2. Cyanoacrylate with lipiodol 1:1.
3. Avoid lateral movements with the needle inside the varicose vein.
4 .Check afferent perforator: contrast or Doppler.
5. Inject 1 ml of cyanoacrylate above the muscle layer.
6. Check occlusion of the varicose vein with Doppler.
Echoendoscopy-guided coil placement technique:
1 .19 G needle.
2 .Coils diameter 20% larger than the varicose vein: 8-20 mm.
3. Remove stylet and push coil with it.
4. Check intravaricose insertion of the coil.
5. As many coils as necessary.
As with EVs, patients with GV and high risk of failure to standard treatment would benefit from placement of a preventive TIPS in the first 72h[7],[8].
Conclusions
1. The treatment of choice in acute bleeding of fundic varices (GOV-2 and IGV-1) is cyanoacrylate injection by conventional endoscopy.
2. Echoendoscopy-guided therapy may be particularly useful in specific situations: poor visibility and retreatment. It reduces cyanoacrylate complications and allows coil release.
3. Combined echoendoscopy-guided treatment (coils + cyanoacrylate) appears to be the most effective and safe strategy today, but well-designed controlled studies are needed to position it as the treatment of choice. This will ensure that in the coming years there will be a stronger position in the recommendations.
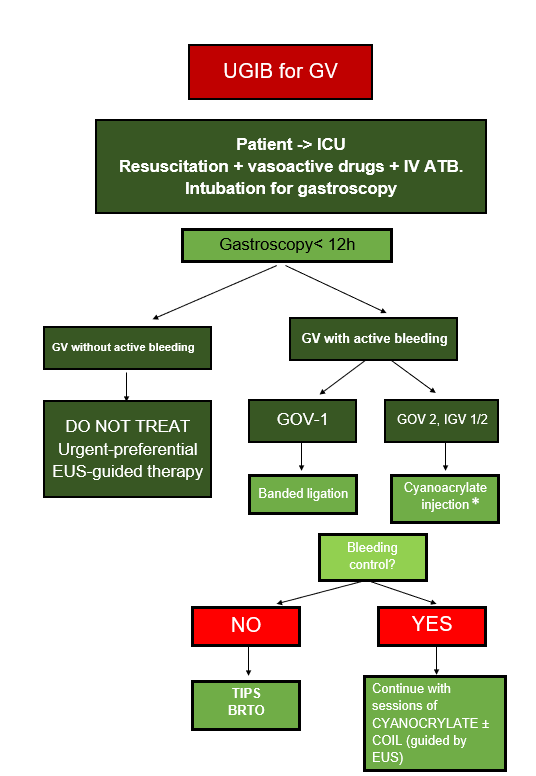
4. Finally, and by way of conclusion, the algorithm of action we follow when there is an active VG haemorrhage in the Virgen Macarena University Hospital is shown graphically (Figure 5).
Figure 5
Algorithm for Acute Hemorrhage from Gastric Varices (GV: Gastric Varices. ICU: Intensive Care Unit. IV ATB: Intravenous Antibiotic Therapy. BRTO: Balloon-occluded Retrograde Transvenous Obliteration). * By standard endoscopy only in case of emergency without an experienced echoendoscopist available. Echoendoscopy-guided treatment (coils+/-cyanoacrylate) is preferable.

 Descargar número completo
Descargar número completo Download full issue
Download full issue